How addiction hijacks the brain
https://www.health.harvard.edu/newsletter_article/how-addiction-hijacks-the-brain
Desire initiates the process, but learning sustains it.
The word "addiction" is derived from a Latin term for "enslaved by" or "bound to." Anyone who has struggled to overcome an addiction — or has tried to help someone else to do so — understands why.
Addiction exerts a long and powerful influence on the brain that manifests in three distinct ways: craving for the object of addiction, loss of control over its use, and continuing involvement with it despite adverse consequences. While overcoming addiction is possible, the process is often long, slow, and complicated. It took years for researchers and policymakers to arrive at this understanding.
In the 1930s, when researchers first began to investigate what caused addictive behavior, they believed that people who developed addictions were somehow morally flawed or lacking in willpower. Overcoming addiction, they thought, involved punishing miscreants or, alternately, encouraging them to muster the will to break a habit.
The scientific consensus has changed since then. Today we recognize addiction as a chronic disease that changes both brain structure and function. Just as cardiovascular disease damages the heart and diabetes impairs the pancreas, addiction hijacks the brain. Recovery from addiction involves willpower, certainly, but it is not enough to "just say no" — as the 1980s slogan suggested. Instead, people typically use multiple strategies — including psychotherapy, medication, and self-care — as they try to break the grip of an addiction.
Another shift in thinking about addiction has occurred as well. For many years, experts believed that only alcohol and powerful drugs could cause addiction. Neuroimaging technologies and more recent research, however, have shown that certain pleasurable activities, such as gambling, shopping, and sex, can also co-opt the brain. Although the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) describes multiple addictions, each tied to a specific substance or activity, consensus is emerging that these may represent multiple expressions of a common underlying brain process.
From liking to wanting
Nobody starts out intending to develop an addiction, but many people get caught in its snare. According to the latest government statistics, nearly 23 million Americans — almost one in 10 — are addicted to alcohol or other drugs. More than two-thirds of people with addiction abuse alcohol. The top three drugs causing addiction are marijuana, opioid (narcotic) pain relievers, and cocaine.
Genetic vulnerability contributes to the risk of developing an addiction. Twin and adoption studies show that about 40% to 60% of susceptibility to addiction is hereditary. But behavior plays a key role, especially when it comes to reinforcing a habit.
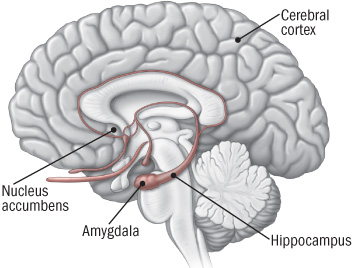
Pleasure principle. The brain registers all pleasures in the same way, whether they originate with a psychoactive drug, a monetary reward, a sexual encounter, or a satisfying meal. In the brain, pleasure has a distinct signature: the release of the neurotransmitter dopamine in the nucleus accumbens, a cluster of nerve cells lying underneath the cerebral cortex (see illustration). Dopamine release in the nucleus accumbens is so consistently tied with pleasure that neuroscientists refer to the region as the brain's pleasure center.
The brain's reward center
Addictive drugs provide a shortcut to the brain's reward system by flooding the nucleus accumbens with dopamine. The hippocampus lays down memories of this rapid sense of satisfaction, and the amygdala creates a conditioned response to certain stimuli. |
All drugs of abuse, from nicotine to heroin, cause a particularly powerful surge of dopamine in the nucleus accumbens. The likelihood that the use of a drug or participation in a rewarding activity will lead to addiction is directly linked to the speed with which it promotes dopamine release, the intensity of that release, and the reliability of that release. Even taking the same drug through different methods of administration can influence how likely it is to lead to addiction. Smoking a drug or injecting it intravenously, as opposed to swallowing it as a pill, for example, generally produces a faster, stronger dopamine signal and is more likely to lead to drug misuse.
Learning process. Scientists once believed that the experience of pleasure alone was enough to prompt people to continue seeking an addictive substance or activity. But more recent research suggests that the situation is more complicated. Dopamine not only contributes to the experience of pleasure, but also plays a role in learning and memory — two key elements in the transition from liking something to becoming addicted to it.
According to the current theory about addiction, dopamine interacts with another neurotransmitter, glutamate, to take over the brain's system of reward-related learning. This system has an important role in sustaining life because it links activities needed for human survival (such as eating and sex) with pleasure and reward. The reward circuit in the brain includes areas involved with motivation and memory as well as with pleasure. Addictive substances and behaviors stimulate the same circuit — and then overload it.
Repeated exposure to an addictive substance or behavior causes nerve cells in the nucleus accumbens and the prefrontal cortex (the area of the brain involved in planning and executing tasks) to communicate in a way that couples liking something with wanting it, in turn driving us to go after it. That is, this process motivates us to take action to seek out the source of pleasure.
Tolerance and compulsion. Over time, the brain adapts in a way that actually makes the sought-after substance or activity less pleasurable.
In nature, rewards usually come only with time and effort. Addictive drugs and behaviors provide a shortcut, flooding the brain with dopamine and other neurotransmitters. Our brains do not have an easy way to withstand the onslaught.
Addictive drugs, for example, can release two to 10 times the amount of dopamine that natural rewards do, and they do it more quickly and more reliably. In a person who becomes addicted, brain receptors become overwhelmed. The brain responds by producing less dopamine or eliminating dopamine receptors — an adaptation similar to turning the volume down on a loudspeaker when noise becomes too loud.
As a result of these adaptations, dopamine has less impact on the brain's reward center. People who develop an addiction typically find that, in time, the desired substance no longer gives them as much pleasure. They have to take more of it to obtain the same dopamine "high" because their brains have adapted — an effect known as tolerance.
At this point, compulsion takes over. The pleasure associated with an addictive drug or behavior subsides — and yet the memory of the desired effect and the need to recreate it (the wanting) persists. It's as though the normal machinery of motivation is no longer functioning.
The learning process mentioned earlier also comes into play. The hippocampus and the amygdala store information about environmental cues associated with the desired substance, so that it can be located again. These memories help create a conditioned response — intense craving — whenever the person encounters those environmental cues.
Cravings contribute not only to addiction but to relapse after a hard-won sobriety. A person addicted to heroin may be in danger of relapse when he sees a hypodermic needle, for example, while another person might start to drink again after seeing a bottle of whiskey. Conditioned learning helps explain why people who develop an addiction risk relapse even after years of abstinence.
ResourcesNational Clearinghouse for Alcohol and Drug Information National Institute on Alcohol Abuse and Alcoholism National Institute on Drug Abuse Substance Abuse and Mental Health Services Administration |
The long road to recovery
Because addiction is learned and stored in the brain as memory, recovery is a slow and hesitant process in which the influence of those memories diminishes.
About 40% to 60% of people with a drug addiction experience at least one relapse after an initial recovery. While this may seem discouraging, the relapse rate is similar to that in other chronic diseases, such as high blood pressure and asthma, where 50% to 70% of people each year experience a recurrence of symptoms significant enough to require medical intervention.
Fortunately a number of effective treatments exist for addiction, usually combining self-help strategies, psychotherapy, and rehabilitation. For some types of addictions, medication may also help.
The precise plan varies based on the nature of the addiction, but all treatments are aimed at helping people to unlearn their addictions while adopting healthier coping strategies — truly a brain-based recovery program.
Benowitz NL. "Nicotine Addiction," The New England Journal of Medicine (June 17, 2010): Vol. 362, No. 24, pp. 2295–303.
Brady KT, et al., eds. Women and Addiction: A Comprehensive Handbook (The Guilford Press, 2009).
Chandler RK, et al. "Treating Drug Abuse and Addiction in the Criminal Justice System: Improving Public Health and Safety," Journal of the American Medical Association (Jan. 14, 2009): Vol. 301, No. 2, pp. 183–90.
Greenfield SF, et al. "Substance Abuse Treatment Entry, Retention, and Outcome in Women: A Review of the Literature," Drug and Alcohol Dependence (Jan. 5, 2007): Vol. 86, No. 1, pp. 1–21.
Koob GF, et al. "Neurocircuitry of Addiction," Neuropsychopharmacology (Jan. 2010): Vol. 35, No. 1, pp. 217–38.
McLellan AT, et al. "Drug Dependence, A Chronic Medical Illness: Implications for Treatment, Insurance, and Outcomes Evaluation," Journal of the American Medical Association (Oct. 4, 2000): Vol. 284, No. 13, pp. 1689–95.
National Institute on Drug Abuse. Drugs, Brains, and Behavior: The Science of Addiction (National Institutes of Health, Aug. 2010).
Polosa R, et al. "Treatment of Nicotine Addiction: Present Therapeutic Options and Pipeline Developments," Trends in Pharmacological Sciences (Jan. 20, 2011): E-publication.
Potenza MN, et al. "Neuroscience of Behavioral and Pharmacological Treatments for Addictions," Neuron (Feb. 24, 2011): Vol. 69, No. 4, pp. 695–712.
Shaffer HJ, et al. "Toward a Syndrome Model of Addiction: Multiple Expressions, Common Etiology," Harvard Review of Psychiatry (Nov.–Dec. 2004): Vol. 12, No. 6, pp. 367–74. *
Stead LF, et al. "Nicotine Replacement Therapy for Smoking Cessation," Cochrane Database of Systematic Reviews (Jan. 23, 2008): Doc. No. CD000146.
Substance Abuse and Mental Health Services Administration. National Survey on Drug Use & Health, 2009.
For more references, please see www.health.harvard.edu/mentalextra.